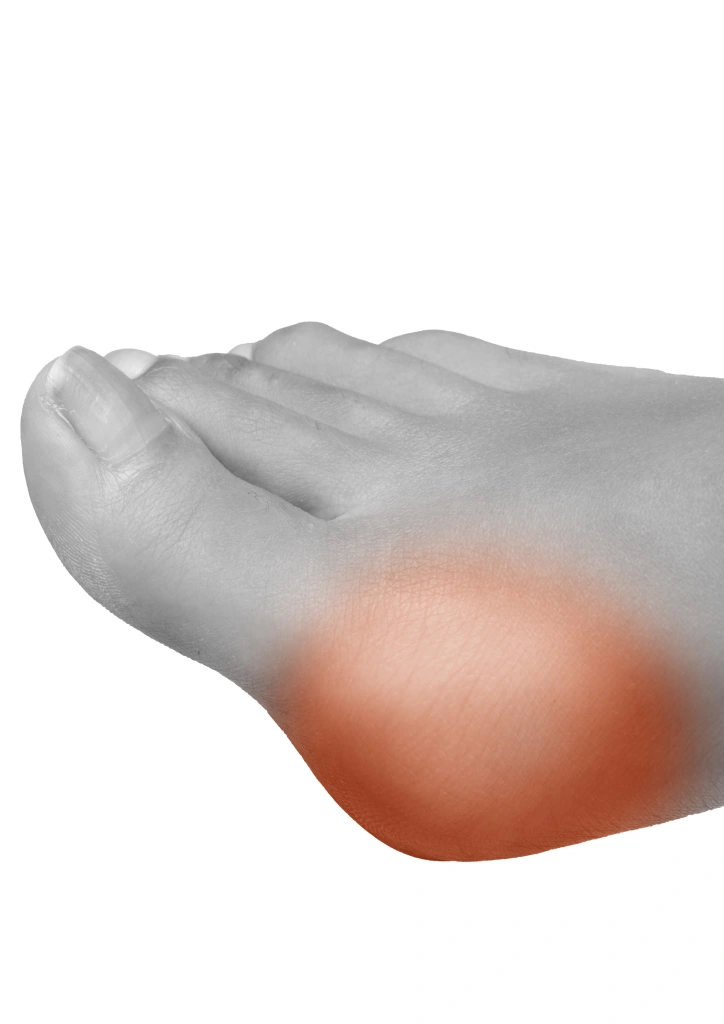
If you are reading this, you are probably already familiar with the discomfort caused by a bunion: persistent pain, difficulty in putting on shoes and limitations in your daily activities. Bunion surgery is designed for:
- Eliminate chronic pain that does not improve with insoles, medication or changes in footwear.
- Restore alignment of the big toe, preventing the deformity from progressing further and compromising other toes.
- Improve function and quality of life: return to walking long distances, playing sports or wearing the footwear of your choice without restrictions.
- Prevent long-term complications such as osteoarthritis, recurrent bursitis and painful corns.
- Optimize foot biomechanics, reducing overloads in neighboring joints (ankle, knee, hip).
In short, the intervention is not only an aesthetic issue; it is the most effective tool to recover your autonomy and prevent further damage in the future.

| Situation | Recommendation |
|---|---|
| Chronic pain that limits daily activities | Operation advised if conservative treatment has failed |
| Rapidly progressive deformity | Early surgical evaluation to avoid irreversible joint damage |
| Associated complications (bursitis, corns, calluses, claw toes) | Surgical correction to prevent skin lesions and overloads |
| Inability to wear regular shoes | High indication to improve quality of life |

Specialist in Percutaneous Foot Surgery
Founder and Medical Director
Based on verified patient feedback
| Phase | Details | Main goal |
|---|---|---|
| SEM -2 → 0 | Medical history, blood work, radiological study in load and 3D scan of the forefoot. | Optimize risk variables and set the surgical strategy. |
| DAY 0 | Regional anesthesia + sedation; surgery 45-90 min; functional dressing and immediate loading with rigid shoe. | Outpatient discharge (97% of cases). |
| SEM 1-2 | Relative rest, cryotherapy, standard analgesics, control teleconsultation. | Maintain pain 2/10 in VAS. |
| SEM 3-6 | Physiotherapy: lymphatic drainage, MLS® laser and passive mobilization. | Restore 80% of joint range. |
| MONTH 2-3 | Wide sports shoes, return to office work and driving. | Walk 5-6 consecutive km without pain. |
| MONTH 4-6 | Start running, paddle tennis or gentle hiking under supervision. | Full physical activity and medical discharge. |

Stabilization Technique without External Fixation
How do we achieve correction without screws and needles?
At Clínica San Román we apply a percutaneous surgery protocol that, in selected cases, allows bone consolidation without the need for metallic implants. This approach is based on three fundamental pillars:
- Precision osteotomies guided by fluoroscopy
We perform millimetrically calculated bone cuts that allow the realignment of the first metatarsal with minimal alteration of the periosteum (membrane that covers the bone and favors natural consolidation). - Specialized functional bandage
We apply a specific compressive bandage that maintains the correction during the first 4-6 weeks, the critical period of initial consolidation. This bandage allows immediate controlled loading, which stimulates bone callus formation. - Progressive offloading protocol
Rigid post-surgical footwear distributes forces in a way that promotes stability without compromising circulation or consolidation.











| Potential risk | Prevention/solution at Clínica San Román |
|---|---|
| Infection ( 1 %) | Sterile technique, antibiotic prophylaxis, protocolized cures. |
| Persistent pain | Multimodal pain management, low power laser and early physiotherapy. |
| Joint stiffness | Active exercises from the 1stweek and specialized manual therapy. |
| Nerve injury (tingling) | Minimal incisions and intraoperative anatomical mapping. |
| Consolidation delay | Metabolic control (vitamin D, blood glucose) and, if necessary, magnetotherapy. |
The key to success lies in an intensive but progressive physiotherapy plan. Our department is equipped with state-of-the-art technologies:
- Sequential pressure therapy to improve venous return and reduce edema.
- Neuromuscular electrostimulation aimed at maintaining the tone of the foot intrinsics.
- Baropodometry platform where we reeducate the footprint and distribute the metatarsal load.
- Myofascial manual therapy that releases adhesions and improves dorsal flexion of the first radius.
88% of our patients are teleworking before the third week and 72% are driving before day 40, thanks to the MIS + ambulatory functional bandaging combination.

References:
Minimally Invasive Foot Ankle Surgery: A Review and a Novel Technique.
- Minimally invasive-percutaneous surgery – recent developments of the foot surgery techniques
- Outcomes and Surgical Strategies of Minimally Invasive Chevron/Akin Procedures
Third-Generation Minimally Invasive Chevron and Akin Osteotomies (MICA) in Hallux Valgus Surgery
- Minimally Invasive Foot and Ankle Surgery: A Primer for Orthopaedic Surgeons
- Minimally invasive surgery: has it come of age?